Malaria research: Scientist industry urged to not underestimate CRISPR’s risks
By IGHI guest blogger Chanice Henry, Editor, Pharma IQ & Pharma Logistics IQ
Similar to new Hollywood feature Rampage, a recent study has urged the life sciences industry not to underestimate the dangers that could hide within CRISPR Cas9.
Although the film has been criticised for wildly exaggerating the capabilities of the gene editing technique, it can be recognised for its effort to draw focus from the excitable buzz around CRISPR Cas9 towards the importance of considering the ethics and dangers associated with the tool.
A recent commentary piece also emphasised the importance of methodically debating the potential outcomes of CRISPR within the task of tackling Malaria.
Malaria is spread by the bite of female mosquitos holding the Plasmodium parasite. Plasmodium falciparum causes life threatening malaria.
Advances made so far
 In the five years to 2015, 17 countries managed to eradicate malaria –including the likes of Senegal and Bolivia. In this period, mortality fell by 50% and incidences fell by 15% – preventing over 6 million deaths.
In the five years to 2015, 17 countries managed to eradicate malaria –including the likes of Senegal and Bolivia. In this period, mortality fell by 50% and incidences fell by 15% – preventing over 6 million deaths.
The World Health Organisation (WHO) recently launched “the world’s first malaria vaccine that has been shown to provide partial protection against malaria in young children.” After establishing efficacy in Phase 3 clinical trials a vaccine implementation programme is due to commence within this year’s immunization projects in Ghana, Kenya and Malawi.
A long way to go
Government spend on malaria prevention has seen a dramatic increase over the past decade. Although, experts note that around $6.5 billion of funding by 2020 will be key to hitting the WHO’s 2030 goal to wipe out malaria in 35 countries and shrink incidents and deaths by 90%.
Statistics claim that malaria still kills one child every two minutes.
Sub-Saharan Africa, as noted by Tanvi Nagpal, housed around 80% of the world’s malaria cases in 2016. “Their high infection rates are compounded by insufficient domestic budgets and struggling health systems.”Reports recently emerged stating of one in four blood banks in certain areas of Sub-Saharan Africa host supplies infected with malaria causing parasites.
Researchers are now turning to CRISPR Cas9 to stop the disease at the source of transmission – the mosquito.
What is CRISPR?
The genome-editing system based on CRISPR-Cas9 is becoming a valuable tool for different applications in biomedical research, drug discovery and human gene therapy by gene repair and gene disruption, gene disruption of viral sequences and programmable RNA targeting. The tool permanently manipulates gene expression by using programmable DNA nuclease and can remove faulty genes from a DNA sequence. (more…)
 Ronald Ross, a British medical doctor of the late-19th and early 20th centuries, was first to identify the mosquito as the winged-insect carrier of malaria-causing parasites. Prior to this breakthrough, bad air (mal aria in Italian) was thought to have been the culprit. Together, Ross and Giovanni Grassi (who’s work, unlike Ross’, was controversially ignored by the Nobel Committee in 1902) uncovered a truth of huge ecological and epidemiological significance and sparked an ongoing international research effort aimed at answering fundamental questions about the processes that drive patterns of human morbidity and mortality caused by diseases carried by mosquitoes.
Ronald Ross, a British medical doctor of the late-19th and early 20th centuries, was first to identify the mosquito as the winged-insect carrier of malaria-causing parasites. Prior to this breakthrough, bad air (mal aria in Italian) was thought to have been the culprit. Together, Ross and Giovanni Grassi (who’s work, unlike Ross’, was controversially ignored by the Nobel Committee in 1902) uncovered a truth of huge ecological and epidemiological significance and sparked an ongoing international research effort aimed at answering fundamental questions about the processes that drive patterns of human morbidity and mortality caused by diseases carried by mosquitoes. Universal health coverage is about ensuring all people can get quality health services, where and when they need them, without suffering financial hardship. No one should have to choose between good health and other life necessities.
Universal health coverage is about ensuring all people can get quality health services, where and when they need them, without suffering financial hardship. No one should have to choose between good health and other life necessities.

 In May of 2017, the BDAU Secure Environment (SE) became the first ISO 27001:2013 (figure 1) and NHS IG Toolkit 100% Level 3 (figure 2) certified research environment in Imperial College. Over the course of 2017, the BDAU SE was successful in completing a further 11 internal and external audits. The 6-month surveillance audit required for retaining ISO 27001 certification was completed with 0 non-conformances. The BDAU now provides advisory to the Imperial College Information Governance Operational Group and the Information Governance Steering Committee for the Department of Surgery and Cancer.
In May of 2017, the BDAU Secure Environment (SE) became the first ISO 27001:2013 (figure 1) and NHS IG Toolkit 100% Level 3 (figure 2) certified research environment in Imperial College. Over the course of 2017, the BDAU SE was successful in completing a further 11 internal and external audits. The 6-month surveillance audit required for retaining ISO 27001 certification was completed with 0 non-conformances. The BDAU now provides advisory to the Imperial College Information Governance Operational Group and the Information Governance Steering Committee for the Department of Surgery and Cancer.
 It is estimated that there are 36.7 million people living with HIV globally with 1.8 million new infections in 2016 alone (1). This number represents an 11% drop in the number of new infections from 2010 . Some might consider this an achievement or a testament to the impact of strategic national and global policies aimed at tackling the epidemic. But in reality, these numbers mask the discrepant pace in the effort to tackle transmission and AIDS-related deaths in countries across the globe. UNAIDS recently reported a steep decline in new infections in sub-Saharan Africa against an alarming increase in the number of new infections in eastern Europe and central Asia in the same period (2). In the UK where the HIV burden is considerably lower, the number of new infections has been steadily falling (3). The reasons for these differences are complex and certain socio-economic factors have the potential to undermine the global effort to tackle transmission.
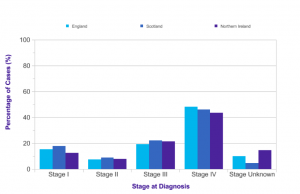
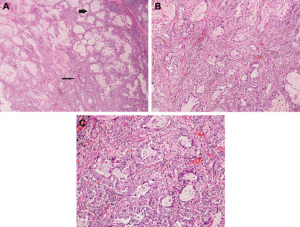
It is estimated that there are 36.7 million people living with HIV globally with 1.8 million new infections in 2016 alone (1). This number represents an 11% drop in the number of new infections from 2010 . Some might consider this an achievement or a testament to the impact of strategic national and global policies aimed at tackling the epidemic. But in reality, these numbers mask the discrepant pace in the effort to tackle transmission and AIDS-related deaths in countries across the globe. UNAIDS recently reported a steep decline in new infections in sub-Saharan Africa against an alarming increase in the number of new infections in eastern Europe and central Asia in the same period (2). In the UK where the HIV burden is considerably lower, the number of new infections has been steadily falling (3). The reasons for these differences are complex and certain socio-economic factors have the potential to undermine the global effort to tackle transmission. The 9th edition of the renowned Osler’s Textbook on the Principles and Practice of Medicine, published in 1921, dedicated only two (out of 1,139) pages to lung cancer, at which point the condition was described as “New Growths in the Lungs”. Almost a hundred years on, the patterns of epidemiology have shifted drastically, and lung cancer now is recognised as a major health problem globally with more than 1.8 million new cases diagnosed every year. It is the second most common cancer diagnosed in the UK for both men and women, with approximately 46,400 new cases in 2014. Unfortunately more than 60% of cases are diagnosed at Stage III and IV (Figure 1 (see below))[1], meaning the tumour has spread outside the lungs and into lymph nodes or other organs.
The 9th edition of the renowned Osler’s Textbook on the Principles and Practice of Medicine, published in 1921, dedicated only two (out of 1,139) pages to lung cancer, at which point the condition was described as “New Growths in the Lungs”. Almost a hundred years on, the patterns of epidemiology have shifted drastically, and lung cancer now is recognised as a major health problem globally with more than 1.8 million new cases diagnosed every year. It is the second most common cancer diagnosed in the UK for both men and women, with approximately 46,400 new cases in 2014. Unfortunately more than 60% of cases are diagnosed at Stage III and IV (Figure 1 (see below))[1], meaning the tumour has spread outside the lungs and into lymph nodes or other organs.