Community Makers: Designing for dementia during the COVID-19 pandemic

People with dementia are some of the most vulnerable, most isolated, and least able to adapt. COVID-19 has therefore made our work with Imperial College’s UK Dementia Research Institute Care Research and Technology Centre all the more urgent.
The Centre develops technologies for a smart ‘Healthy Home environment‘, supported by remote clinical monitoring, to improve the lives of people affected by dementia and further our understanding of this common disease.
The technology aims to make an impact in a number of ways, including early identification of infection, preventing falls, understanding the relationship between sleep and dementia symptoms, and predicting and managing agitation and difficult behaviours. All with the goal of reducing hospitalisation and improving the resilience of at-home care.
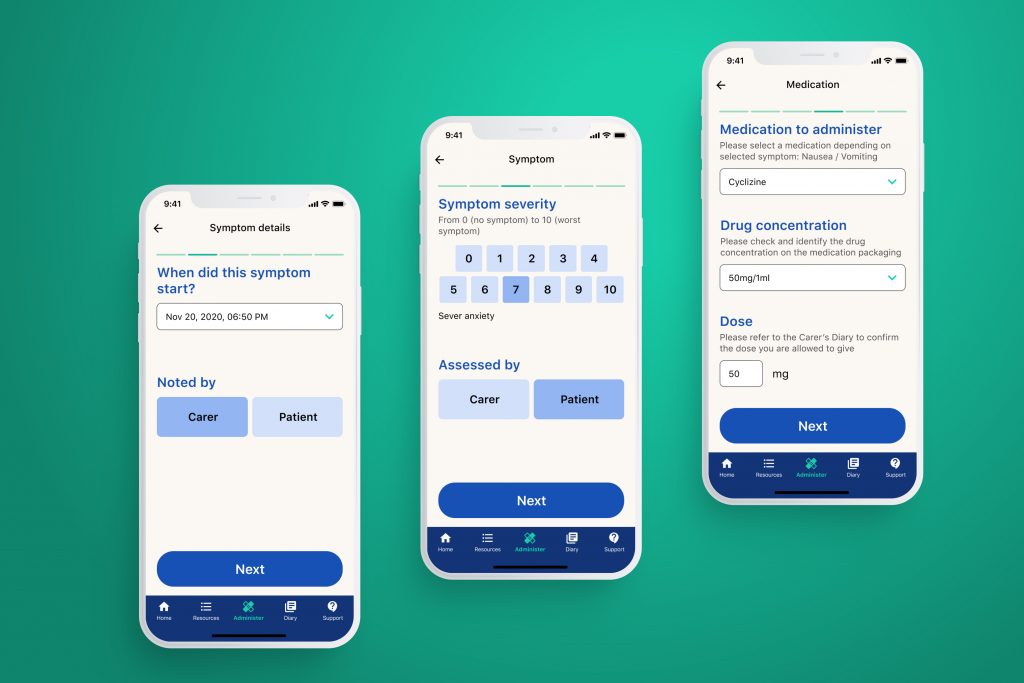
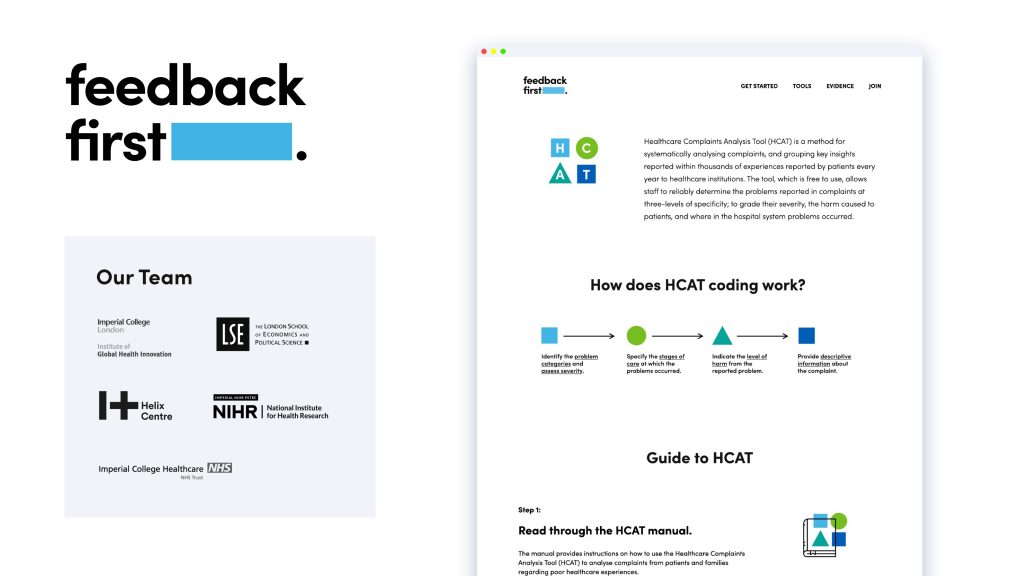
Our team at the Helix Centre is using our human-centred design methods to put patient and carer needs at the core of everything the Centre does. This includes designing the monitoring dashboard to optimise the relationship between the monitoring team and the at-home participants, and creating a companion app for people to access their data and assist with the daily tasks of caring for someone with dementia.
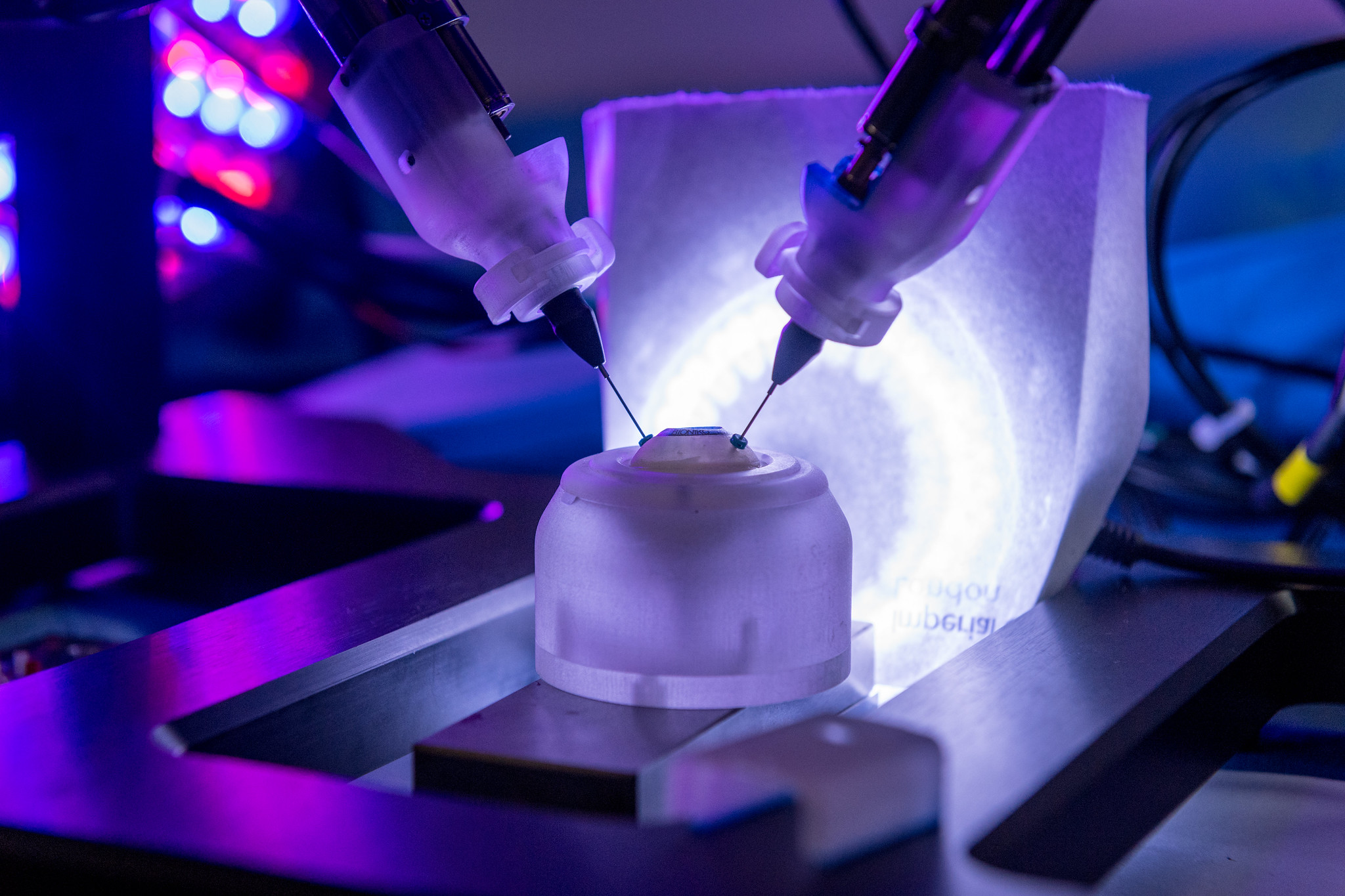
We’re also working with science and engineering labs throughout Imperial College London and the University of Surrey to inform the creation of new devices. These range from at-home UTI diagnostics with the synthetic biology team, a smart speaker voice agent to assist in care tasks, and radar sensors and wearables to help monitor behaviour within the house.
Adapting during COVID-19
Our co-design process relies on spending time with people, in their homes, getting to know their lives, aspirations and needs. In response to COVID-19 restrictions, we moved this process online, using video conferencing software to hold regular co-design sessions with a surprising increase in engagement and richness of connection.
Out of this came an idea to help reduce isolation for people with dementia and their family carers during the pandemic. We joined forces with the Alzheimer’s Society Innovation team and the Association of Dementia Studies at the University of Worcester to explore how technology could play a role for this vulnerable and extremely isolated group.
Families living with dementia rely heavily on community support groups, visiting friends, neighbours, carers and community services to help manage the heavy burden of caring for someone with dementia in their own home. All of this support evaporated when lockdown measures were imposed, and the isolation has had a profound impact on the wellbeing and resilience of carers. The alternative of residential care homes has been even less attractive during lockdown for well-documented reasons.
Through this collaboration, we identified a need to help existing groups in the community to go digital and move their support online, so that they could continue to reach their members.
Supporting people affected by dementia
We developed Community Makers, a digital resource to help groups set up local online networks to replace the face-to-face meetings that provided key support pre-COVID. This includes a knowledge exchange network that meets online monthly to share experiences and advice, and a library of creative ideas to inspire groups with different approaches to digital involvement.
We also have a Slack workspace, currently consisting of 64 community organisers representing groups from Scotland, Wales and England, rural and urban settings, and including groups focussing on ethnic and minority populations. Groups within the network vary in size from supporting over 150 people with dementia to new groups just setting up. One example is Dementia Matters Here(forshire), established during the pandemic as a digital-first group on the back of our Community Makers collaboration.
If you’re part of a support group that you want to bring online, you can head to our website and use our guide to getting started. We look forward to welcoming you to our growing community.
Community Makers has been led by Matthew Harrison, Senior designer in Helix Centre, supported by Alice Blencowe and Lenny Naar.
 It’s been almost a month since Imperial PhD student Sam Tukra won IGHI’s
It’s been almost a month since Imperial PhD student Sam Tukra won IGHI’s  By Laura Braun, co-founder of Capta, 2018/19 winners of IGHI’s Student Challenges Competition
By Laura Braun, co-founder of Capta, 2018/19 winners of IGHI’s Student Challenges Competition





 Every Christmas, researchers from IGHI’s
Every Christmas, researchers from IGHI’s