One year on – how our researchers have responded to the pandemic

“We’re in this together.” One year ago, on 11th March 2020, the World Health Organization declared COVID-19 a global pandemic.
Back then, little over 100,000 cases had been reported globally. Today that number is 1,000 times greater and growing ceaselessly.
With a barely known virus rippling across the world, so too did fear and uncertainty spread as the WHO Director-General addressed all people and nations to make the declaration. Shifting the focus from COVID-19 to people and unity, Dr Tedros also sparked glimmers of optimism by emphasising that innovation and learning would be integral to saving lives and minimising the impact of the pandemic.
Innovation is the beating heart of IGHI, and we’re proud of our community that has joined this long and winding path of discovery in many different ways. A year on, our people reflect on their COVID-19 response journeys and impart the lessons they’ve learned along the way.
Read their stories below.
Tracking COVID-19 past and present – the REACT study
In April 2020 we launched the biggest and most comprehensive study of home coronavirus testing. With colleagues across the College, Imperial College Healthcare NHS Trust, and Ipsos MORI, the REACT programme has been testing hundreds of thousands of people across England every month to track infections past and present. Alongside understanding how many people are currently infected, REACT is identifying people who are most at risk of infection while offering a range of other important insights, such as antibody responses to vaccination. The programme has also worked closely with members of the public to ensure that the research is guided by people’s needs.
This work has been instrumental in the monitoring of England’s epidemic and offers robust, timely evidence on the evolving situation, which is continuing to shape the government’s response.
“One phrase has dominated Government pronouncements on the roadmap out of lockdown: ‘Data, not dates,’” said Professor Ara Darzi, REACT programme sponsor and co-director of IGHI. “And rightly so. The Covid crisis has caused terrible suffering, wrecking lives and livelihoods. But unless we understand it, we cannot defeat it.
“Among the most pressing questions over the last year have been how many people are currently infected with the virus, and how far has it spread through the population? REACT has been a key element of the effort to answer these questions, providing among the most accurate and up-to-date data on its progression across England.
“By regularly testing 160,000 randomly selected people every month, the study has played a vital role in informing the Government’s decision over when to impose lockdown and when to lift it.
“In doing so it has proved the central importance of accurate data gathering to control this and any future pandemic. We forget this lesson at our peril.”

Designing for dementia – Community Makers
Social distancing measures have helped keep the virus at bay, but not without cost. The loneliness and isolation that come with keeping people apart are negatively impacting people’s wellbeing, particularly so for those who depend on support from others in their everyday lives, such as people with dementia.
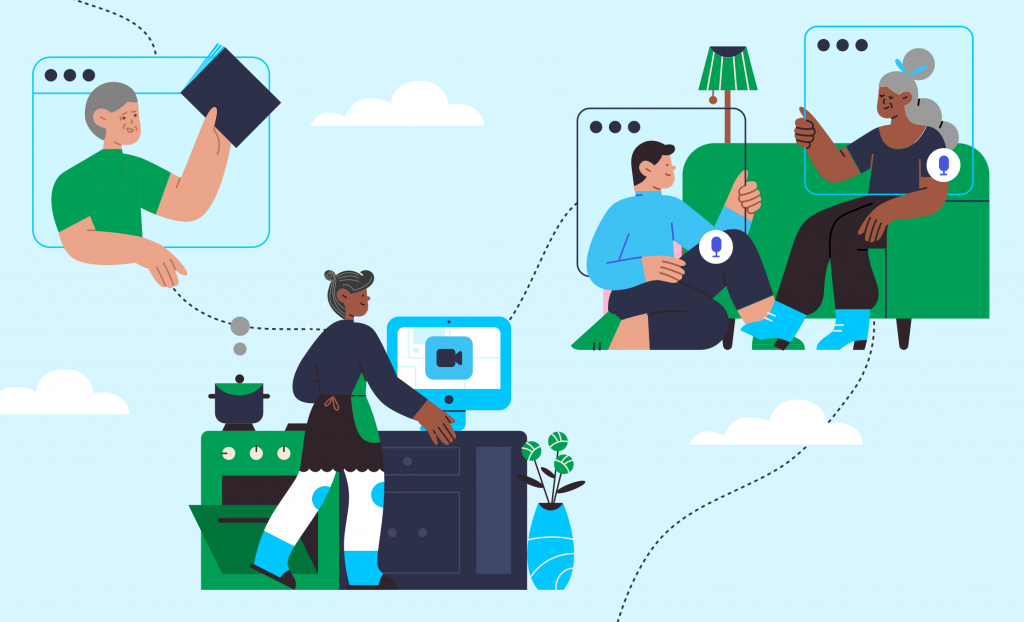
In response to this issue, our Helix Centre partnered with collaborators to develop a digital resource to help community groups create online networks as a way to maintain support and connection for people affected by dementia. Called Community Makers, the initiative is also building a toolkit of creative ideas for digital involvement, including how to reach people who may not have access to technology.
“Community Makers was a project that addressed a real-time need we saw in the people we were working with through our dementia research,” said Matt Harrison, senior designer at IGHI’s Helix Centre and project lead at Imperial. “People with dementia were some of the least able to adapt to lockdown measures and keep themselves isolated, yet very vulnerable to COVID.
“Collaborating daily with colleagues I have never met in person, at Alzheimer’s Society and University of Worcester, it has been inspiring to work with community groups across the country and see how they have adapted to using digital tools to support their members, and see how technology has evolved to match the need. However, the need is still not met, and there is much more to be done. The post-COVID world will be made up of the best of in-person and digital connections, and we are now seeking funding to help facilitate that change.”
Read more about Community Makers here.
Monitoring people’s changing attitudes and behaviours
Washing our hands regularly, taking public transport, avoiding meeting people outside of our household – many of the things we do affect our risk of COVID-19. Public health measures and campaigns have been designed to encourage people to behave in ways that reduce this risk, but how well are people sticking to them? And how are people’s attitudes in relation to the crisis changing over time?
Launched in March 2020 with YouGov, our ongoing COVID-19 health behaviour study is the largest of its kind, surveying thousands of people across the globe every month – half a million in total to date – to understand how citizens are responding to the pandemic. By making the findings freely available, and collaborating with a range of partners, our work is enabling decision-makers to tailor their response based on evidence.
“The stories that emerged, their common threads and their remarkable differences have helped many scientists, public health authorities, members of the press, government leaders and the public to come to grips with many of the driving forces behind the spread of COVID-19,” said Sarah P Jones, project co-creator and doctoral researcher at IGHI.
“When I look back across the year I’m struck by not the divisions sown between us, but by the overwhelming cooperation the world has generated.
“At the beginning of the pandemic I saw every new announcement as a rule, a constraint or a liberty taken away.
“But starting from the very first time YouGov returned our global survey results, I realised something incredible was happening in the world.
“Every hand washed, every mask worn, every metre of distance we placed between ourselves and others have been a gesture towards each other, a signal of respecting one another’s safety.
“I personally cannot wait to get back to hugging, to hearing stories in person and to caring for those I love who are still far away.
“But as we emerge from this cocoon the question on many peoples’ minds should not be “How can we get back to normal?” but rather “Is there anything we cannot accomplish together?”
Find out more about the behaviour tracker here.
Understanding the impact of the COVID-driven digital shift in primary care
Digital technologies have been poised to transform the delivery of health care for some time. When the pandemic hit, their promise was quickly put to the test as health systems were forced to shift much of their care from in-person to remote delivery.
Switching from face-to-face consultations to phone calls and video meetings has enabled services to continue while keeping both patients and healthcare staff safe. But what has been the impact for patients and professionals? Our international InSIGHT study has been working with global collaborators to explore this in primary care, using a survey to gather the perspectives of thousands of GPs across 20 countries.
“We were pleased to hear that GPs identified a range of benefits, including reducing COVID-19 transmission risks, guaranteeing access and continuity of care, greater efficiency, faster access to care, and improved convenience for patients,” said study lead Dr Ana Luisa Neves, Advanced Research Fellow and Associate Director of our NIHR Imperial Patient Safety Translational Research Centre.
“We also learnt about the main challenges of using remote care, faced by both patients and doctors – digital exclusion from lacking access to technology, clinical uncertainty, potential delays in diagnosis and treatment, and unsuitability for certain types of consultations.
“The work also highlighted other challenges such as the lack of formal guidance, higher workloads, and technical difficulties. Unsurprisingly, digital exclusion and the potential to entrench existing health inequities were among the major concerns of the participants.
“We believe that listening to the GPs’ experience during the pandemic is especially valuable to understand how digital remote care can be safely delivered in the future. We hope we can learn together from this massive real-life experiment and use this opportunity to take the best technology has to offer and change primary care for the better.”
Find out more about InSIGHT here.

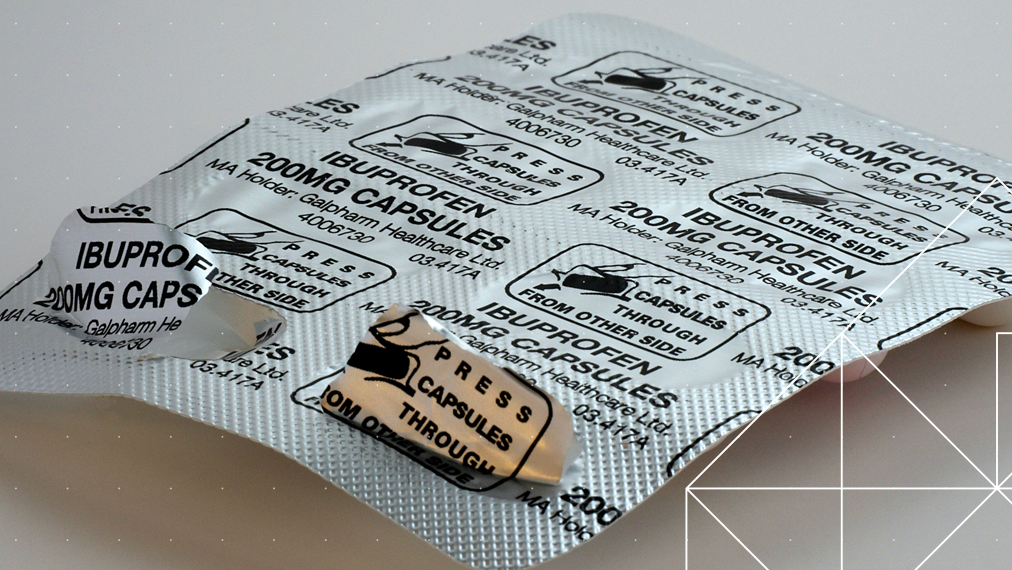 When we’re having issues with our health, as well as visiting the doctor or hospital, one option we have is purchasing over-the-counter (OTC) medicines to treat ourselves at home.
When we’re having issues with our health, as well as visiting the doctor or hospital, one option we have is purchasing over-the-counter (OTC) medicines to treat ourselves at home. My move from paediatric intensive care nursing to research nursing was a natural and exciting one. Both roles require excellent communication skills, whether that’s talking to patients and their families, or members of the multidisciplinary team.
My move from paediatric intensive care nursing to research nursing was a natural and exciting one. Both roles require excellent communication skills, whether that’s talking to patients and their families, or members of the multidisciplinary team.
 IGHI is home to a team of staff who are skilled and passionate about their roles. Our talented people are the reason we’re able to tackle some of the most pressing global health challenges through cutting-edge innovation.
IGHI is home to a team of staff who are skilled and passionate about their roles. Our talented people are the reason we’re able to tackle some of the most pressing global health challenges through cutting-edge innovation.
 As we approach Christmas and the end of a challenging year, it’s a time to reflect on our progress and the changes we’d like to see.
As we approach Christmas and the end of a challenging year, it’s a time to reflect on our progress and the changes we’d like to see.