By Dr Ryan Li, Adviser, Imperial College London, Global Health and Development Group
 Universal health coverage is about ensuring all people can get quality health services, where and when they need them, without suffering financial hardship. No one should have to choose between good health and other life necessities.
Universal health coverage is about ensuring all people can get quality health services, where and when they need them, without suffering financial hardship. No one should have to choose between good health and other life necessities.
As part of World Health Day, Dr Ryan Li from the Global Health & Development Group who is an advisor for the International Decision Support Initiative (iDSI), which supports countries to get the best value for money from health spending, reflects on a visit to Vietnam and the principles for developing clinical quality standards in Low and Middle Income Countries (LMICs):
I remember very vividly two of the hospitals I visited in Vietnam, during my first field trip as a global health advisor for iDSI. In a central hospital in Hanoi, I saw an acute stroke centre that was spotlessly clean and gleaming with the latest equipment, with specialised stroke clinicians offering a range evidence-based treatments matching Western standards. In contrast, in a district hospital a mere two hours away from the capital city, I saw an elderly woman with suspected stroke who had been hospitalised for two weeks, seemingly not getting any better and not receiving any meaningful treatment (and there was no way to confirm the diagnosis as no brain imaging could be done). There was no question as to which hospital I would choose, if I could, if a relative or I were unfortunate to have a stroke.
The reality is that for most people, there is no choice – those who have the means to access the better hospitals, perhaps simply because they live closer to the city, likely get better treatment. This is unfair. Universal health coverage (UHC) is only truly universal if everyone has fair access to good quality health services, irrespective of where they live, what facilities they have access to, their education, income, religion or ethnic background.
Variation in quality is not a phenomenon unique to Vietnam, but is a reality in health systems across the world – even in relatively well-resourced and well-performing UHC systems such as the UK National Health Service. Some variation in quality may be acceptable, but one reason why unacceptable variation occurs is that there is a lack of clarity across the system about what is best practice.
Quality standards
In a bid to address this variation, the National Institute for Health and Care Excellence (NICE) in the UK introduced Quality Standards (QS): concise sets of statements that describe what is best practice in a given disease area (drawn from existing evidence based guidelines). For instance, what kinds of and how many antenatal checks a pregnant woman should ideally receive; sets out the practical steps required to achieve improvement; and most importantly quantifies the improvement. In essence, QS brings everyone together to identify the top five or 10 things that need improving nationally; and focus efforts towards raising standards in those areas.
Since 2012, iDSI has been working with India, China, Vietnam and Thailand to develop and implement QS as ways of tackling inequalities in healthcare quality; and to raise overall standards in key areas such as antenatal and maternal health, non-communicable diseases (stroke, hypertension, and diabetes) and antimicrobial resistance. We have drawn on our UK and international experience to create a guide to QS, which is now available in the resources section of the iDSI website and on our iDSI Knowledge Gateway.
Thailand, long seen as a success story of UHC, also recognises unacceptable variation in quality among public healthcare providers. In particular, there is now a push to raise and standardise quality in health promotion and disease prevention, beginning with QS in antenatal care. I was privileged to be invited as an international expert to observe and advise on this process. The discussions I heard among policymakers, clinicians and grassroots health volunteers were so rich that I can already anticipate insights and lessons that will go into the next version of the QS guide.
The enthusiasm and expertise of the stroke clinicians I met in the central hospital in Vietnam was unquestionable; the challenge is to sustain those excellent standards of practice and to ensure that all healthcare services across a country can reach those standards. iDSI’s vision is that everyone has fair access to quality healthcare, and we hope that our efforts in introducing and localising the QS model is a small step in the right direction.
Read Taking part in the UHC conversation in full
 Today mark’s World Blood Donor Day – an event to celebrate and thank volunteers the world over, who generously donate blood to support life-saving care and to raise awareness of the continued need for donations of blood and blood products to support high quality safe care for patients who need it most.
Today mark’s World Blood Donor Day – an event to celebrate and thank volunteers the world over, who generously donate blood to support life-saving care and to raise awareness of the continued need for donations of blood and blood products to support high quality safe care for patients who need it most. Making motherhood safe is a human rights imperative. In the last 20 years, a steady decline has been observed in maternal mortality rates worldwide, but much more needs to be done: nearly 300,000 women still die every year because of pregnancy or childbirth-related complications (1). This means that a mother dies every two minutes.
Making motherhood safe is a human rights imperative. In the last 20 years, a steady decline has been observed in maternal mortality rates worldwide, but much more needs to be done: nearly 300,000 women still die every year because of pregnancy or childbirth-related complications (1). This means that a mother dies every two minutes. This
This  Ronald Ross, a British medical doctor of the late-19th and early 20th centuries, was first to identify the mosquito as the winged-insect carrier of malaria-causing parasites. Prior to this breakthrough, bad air (mal aria in Italian) was thought to have been the culprit. Together, Ross and Giovanni Grassi (who’s work, unlike Ross’, was controversially ignored by the Nobel Committee in 1902) uncovered a truth of huge ecological and epidemiological significance and sparked an ongoing international research effort aimed at answering fundamental questions about the processes that drive patterns of human morbidity and mortality caused by diseases carried by mosquitoes.
Ronald Ross, a British medical doctor of the late-19th and early 20th centuries, was first to identify the mosquito as the winged-insect carrier of malaria-causing parasites. Prior to this breakthrough, bad air (mal aria in Italian) was thought to have been the culprit. Together, Ross and Giovanni Grassi (who’s work, unlike Ross’, was controversially ignored by the Nobel Committee in 1902) uncovered a truth of huge ecological and epidemiological significance and sparked an ongoing international research effort aimed at answering fundamental questions about the processes that drive patterns of human morbidity and mortality caused by diseases carried by mosquitoes. Universal health coverage is about ensuring all people can get quality health services, where and when they need them, without suffering financial hardship. No one should have to choose between good health and other life necessities.
Universal health coverage is about ensuring all people can get quality health services, where and when they need them, without suffering financial hardship. No one should have to choose between good health and other life necessities.

 It is estimated that there are 36.7 million people living with HIV globally with 1.8 million new infections in 2016 alone (1). This number represents an 11% drop in the number of new infections from 2010 . Some might consider this an achievement or a testament to the impact of strategic national and global policies aimed at tackling the epidemic. But in reality, these numbers mask the discrepant pace in the effort to tackle transmission and AIDS-related deaths in countries across the globe. UNAIDS recently reported a steep decline in new infections in sub-Saharan Africa against an alarming increase in the number of new infections in eastern Europe and central Asia in the same period (2). In the UK where the HIV burden is considerably lower, the number of new infections has been steadily falling (3). The reasons for these differences are complex and certain socio-economic factors have the potential to undermine the global effort to tackle transmission.
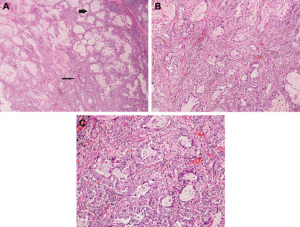
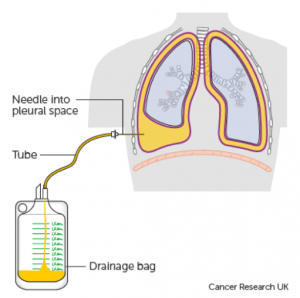
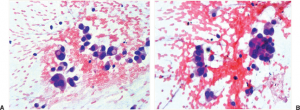
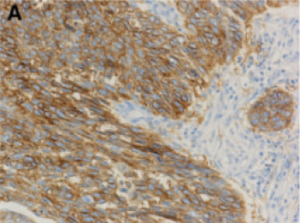
It is estimated that there are 36.7 million people living with HIV globally with 1.8 million new infections in 2016 alone (1). This number represents an 11% drop in the number of new infections from 2010 . Some might consider this an achievement or a testament to the impact of strategic national and global policies aimed at tackling the epidemic. But in reality, these numbers mask the discrepant pace in the effort to tackle transmission and AIDS-related deaths in countries across the globe. UNAIDS recently reported a steep decline in new infections in sub-Saharan Africa against an alarming increase in the number of new infections in eastern Europe and central Asia in the same period (2). In the UK where the HIV burden is considerably lower, the number of new infections has been steadily falling (3). The reasons for these differences are complex and certain socio-economic factors have the potential to undermine the global effort to tackle transmission. The 9th edition of the renowned Osler’s Textbook on the Principles and Practice of Medicine, published in 1921, dedicated only two (out of 1,139) pages to lung cancer, at which point the condition was described as “New Growths in the Lungs”. Almost a hundred years on, the patterns of epidemiology have shifted drastically, and lung cancer now is recognised as a major health problem globally with more than 1.8 million new cases diagnosed every year. It is the second most common cancer diagnosed in the UK for both men and women, with approximately 46,400 new cases in 2014. Unfortunately more than 60% of cases are diagnosed at Stage III and IV (Figure 1 (see below))[1], meaning the tumour has spread outside the lungs and into lymph nodes or other organs.
The 9th edition of the renowned Osler’s Textbook on the Principles and Practice of Medicine, published in 1921, dedicated only two (out of 1,139) pages to lung cancer, at which point the condition was described as “New Growths in the Lungs”. Almost a hundred years on, the patterns of epidemiology have shifted drastically, and lung cancer now is recognised as a major health problem globally with more than 1.8 million new cases diagnosed every year. It is the second most common cancer diagnosed in the UK for both men and women, with approximately 46,400 new cases in 2014. Unfortunately more than 60% of cases are diagnosed at Stage III and IV (Figure 1 (see below))[1], meaning the tumour has spread outside the lungs and into lymph nodes or other organs.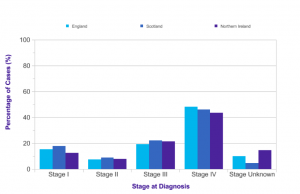
 Antibiotics are a powerful resource that allows us to safely perform surgery, treat cancer with chemotherapy, and recover from infections that over 100 years ago would have killed even the fittest among us.
Antibiotics are a powerful resource that allows us to safely perform surgery, treat cancer with chemotherapy, and recover from infections that over 100 years ago would have killed even the fittest among us.