Acute Hepatitis
Distinguish acute and chronic hepatitis.
Liver disease lasting less (acute) or more (chronic) 6 months.
Describe the natural history of hepatitis.
Acute hepatitis > chronic hepatitis > cirrhosis
Name the 2 commonest causes of acute hepatitis.
- Drugs
- Viruses
Name 5 viruses which cause acute hepatitis.
HAV, HBV, HCV, HDV and HEV
Name one drug that causes an acute hepatitis.
Paracetamol
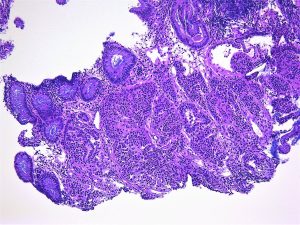
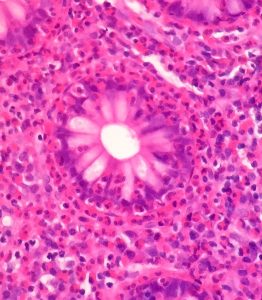
Describe the characteristic histological features of an acute hepatitis.
Spotty (lobular) hepatocyte necrosis and inflammation
Chronic Hepatitis
Name the 3 causes of a chronic hepatitis
- Viruses
- Drugs
- Autoimmune
Define grade with reference to chronic hepatitis.
The activity of the inflammation (portal, interface and lobular).
Define stage with reference to chronic hepatitis.
The degree of fibrosis ranging from portal tract expansion through bridging fibrosis to nodule formation (= cirrhosis).
Name the scoring system for grading and staging chronic hepatitis that you use in your hospital.
Modified HAI (Ishak) / METAVIR
Viral Hepatitis
Name 3 viruses which cause chronic hepatitis.
HBV, HCV and HDV (causes co-infection / superinfection with HBV).
Describe the characteristic histological feature of chronic hepatitis B.
Ground glass cells, immunopathic hepatocyte damage
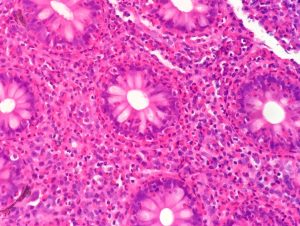
Describe the 3 characteristic histological features of chronic hepatitis C.
Inflammatory bile duct damage, lymphoid follicle formation, fatty change (Genotype 3).
Describe the characteristic histological feature of hepatitis D.
Cytopathic hepatocyte damage
Auto-immune Hepatitis
List the main clinical features.
Younger women, often associated with other autoimmune diseases
Classify auto-immune hepatitis.
Type 1 Associated with smooth muscle actin antibodies in adults (and the commonest one we see).
Type 2 associated with liver-kidney microsomal antibodies, commoner in children
Describe the 2 characteristic histological features of auto-immune hepatitis.
Marked, especially interface, inflammation and prominent plasma cells.
Be aware of the existence of overlap syndromes.
With PBC and PSC.
Drug induced hepatitis
and Drug Induced Liver Injury (DILI)
Describe the range of liver diseases that can be caused by a drug.
‘Any kind of liver disease can be caused by a drug”.
Describe 5 characteristic histological features of a drug-induced hepatitis.
Fatty change, eosinophils, granulomas, cholestasis, dropout
Name one drug which causes a chronic hepatitis.
Isoniazid
Fatty Liver Disease:
Describe the natural history of fatty liver hepatitis.
Fatty change> fatty liver hepatitis > cirrhosis
Describe the 2 morphological types of fatty change.
Small droplet (microvesicular) and large droplet (macrovesicular)
List the 2 common causes of each type of fatty change.
Small droplet: Drugs (e.g. sodium valproate) and pregnancy.
Large droplet: Alcohol and Diabetes (insulin resistance).
List 4 other causes of large droplet fatty change.
Drugs (e.g. steroids), viruses (HCV), starvation and other metabolic diseases (e.g. Wilson’s Disease).
Describe the 4 key histological features of a fatty liver hepatitis.
All changes most marked in Zone 3: ballooning (with or without Mallory-Denk bodies), inflammation (lymphocytic and / neutrophilic, pericellular fibrosis.
Know which histological feature may help distinguish alcoholic from non-alcoholic fatty change.
Nuclear vacuolation which is associated with insulin resistance.
Know the associations of nuclear vacuolation.
Physiological: childhood and young adults.
Pathological: insulin resistance, Wilson’s Disease and glycogen storage diseases.
Name the 2 commonest causes of a fatty liver hepatitis.
Alcohol and Diabetes / insulin resistance (= Non-Alcoholic Steato-Hepatitis)
These 3 stages may co-exist
Name one drug that causes a fatty liver hepatitis.
Tamoxifen
Name the scoring system for grading and staging chronic hepatitis that you use in your hospital.
Nash Activity Score (NAS) and Stage
Primary biliary cholangitis (PBC)
List the main clinical features.
Middle aged, females
The presence of anti-mitochondrial antibodies is the key diagnostic test.
Describe the key histological feature.
Inflammatory destruction of bile ducts often associated with granulomas.
General features of chronic cholestatic liver disease (see below).
Progressive portal fibrosis but less than half are cirrhotic at presentation
Primary sclerosing cholangitis (PSC)
List the key clinical features.
Younger men
Associated with ulcerative colitis.
Increased risk of cholangiocarcinoma.
Imaging is the key diagnostic test,
Describe the key histological feature.
Fibrotic destruction of bile ducts.
Progressive portal fibrosis.
Involves mainly the extrahepatic bile ducts.
List the diseases that cause bile duct loss.
- PBC
- PSC
- Drug-induced liver disease e.g. ketamine
- Chronic liver transplant rejection
- Graft versus Host Disease etc.
Know the general features of chronic cholestatic liver disease and which special stains are needed to demonstrate them.
- Bile duct loss
- Proliferation of intermediate-type hepatocyte progenitor cells.
- Accumulation of copper and copper associated protein in periportal hepatocytes.
- Ballooning degeneration of periportal hepatocytes (with or without Mallory-Denk bodies).
1 and 2 confirmed on CK7 staining.
Copper-associated protein: metallothionine
Copper: rubeanic acid
List the features which assess the active damage of biliary tract disease.
- bile duct inflammation
- interface hepatitis
List the features which assess the chronic damage of biliary tract disease.
- portal fibrosis
- interlobular bile duct loss
- deposition of copper associated protein.
Wilson ’s disease
List the main clinical features.
Associated with neurological problems (“hepato-lenticular degeneration”) and eye involvement (Kayser-Fleisher rings).
Should always be considered in younger patients with unexplained liver disease.
Describe the underlying pathophysiology
Autosomal recessive with no dominant mutation.
Failure of copper excretion by hepatocytes into the biliary system due the failure to express a transporter protein
Describe the range of histological features.
From fatty liver hepatitis to chronic hepatitis.
Increased copper or copper associated protein can only be demonstrated, histologically, in half of cases:
The gold standard is liver copper measurement.
NB Copper also increased in chronic biliary tract diseases but not the same extent.
Haemochromatosis
List the main clinical features
Presents in adults but in men earlier than in women.
Describe the underlying pathophysiology
Autosomal recessive with a single dominant mutation (HFe)
Increased iron absorption from the gut. NB There is no method for excreting iron
Describe the key histological features.
Iron deposition in hepatocytes starting in the periportal hepatocytes and then spreading to the rest of the lobule.
Progressive portal fibrosis.
Be able to distinguish this from other causes of iron overload.
Chronic anaemia, also, leads to increased iron absorption from the gut and deposition in hepatocytes.
Blood transfusion leads to iron deposition in Kupffer cells and does not, usually, lead to fibrosis.
Alpha-1 antitrypsin deficiency
List the key clinical features
Associated with emphysema
Describe the key histological feature.
dPAS positive globules in periportal hepatocytes.
IgG Related Disease (IgG4)
List the main clinical features
Often part of systemic disorder
Often involves the hepato-biliary (and pancreatic) system producing, e.g.:
- A mass lesion in the liver
- A PSC like disease
List the 3 key histological features.
- Increased numbers of IgG4 expressing plasma cells.
- Storiform fibrosis
- Vasculo-obliterative lesions
Granulomas
Know a classification of granulomas in the liver:
- Aetiolgical
- Practical
- Where you know the cause:
e.g. see a schistosome egg or acid-fast bacilli
- Where you can have an educated guess:
e.g. Associated with bile duct damage (PBC) or portal based, fibrotic granuloma with little associated inflammation (Sarcoid) or associated with other features suggesting DILI.
- The rest!
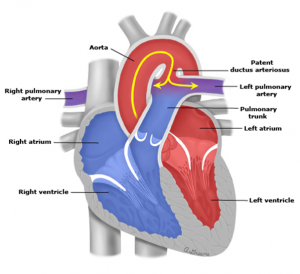
Vascular Diseases of the Liver
Describe the clinical associations and key histological features of the main vascular diseases of the liver.
- Budd Chiari Syndrome
Thromboses of hepatic vein / branches etc.
Associated with pro-thrombotic states
Marked congestion, with extravasation of red cells onto hepatocytes, and patent central veins.
- Veno-occlusive disease
Fibrotic obliteration of portal vein branches.
Associated with azathioprine, radiation and Jamaican bush tea
- Sinusoidal obstruction syndrome.
Sinusoidal damage with congestion and haemorrhage,
Associated with chemotherapy,
- Primary portal hypertension.
Obliteration of hepatic vein branches and sinusoidal herniation.
- Nodular regenerative hyperplasia.
Regenerative nodules but no fibrosis.
Associated with systemic diseases
Cirrhosis
Define cirrhosis.
End stage liver disease:
- involving the whole liver,
- associated with fibrosis,
- nodules of regenerating hepatocytes and
- shunting of blood (intrahepatic and extrahepatic)
List the 3 commonest causes of cirrhosis
- Viral hepatitis
- Alcoholic liver disease
- Non- alcoholic fatty liver disease (NAFLD)
List 4 other causes of cirrhosis.
- PBC
- PSC
- DILI
- Hemochromatosis
Know how to classify cirrhosis.
- According to the aetiology
- According to the sizes of the nodules
Micronodular (smaller than a normal liver lobule) – alcohol
Macronodular (bigger than a normal liver lobule) – viral hepatitis
Mixed
List 3 complications of cirrhosis.
- Portal hypertension.
- Liver failure
- Liver cell cancer
Read Medical Liver Biopsies for Trainees. in full