Assessing risk for healthcare workers during the Covid-19 pandemic
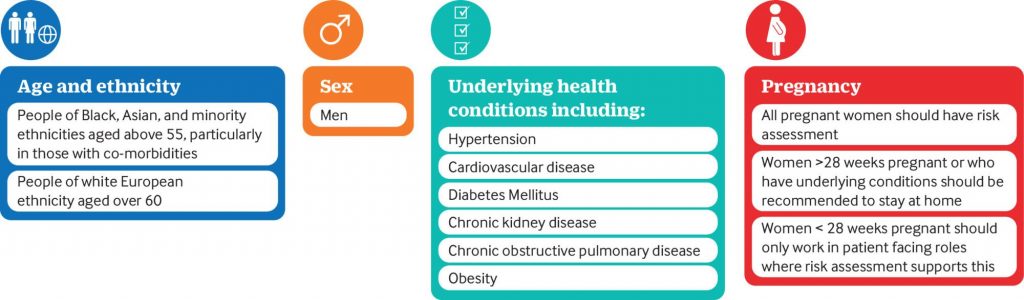
In March 2020, the World Health Organization classified Covid-19 as an international pandemic. Initial guidance from many organisations identified people who might be more vulnerable to covid-19, based on knowledge of those known to be most susceptible to adverse outcomes from the influenza virus. Health conditions divided individuals into those who are “extremely vulnerable,” for whom shielding is required, and those at “increased risk of severe illness.”
In a paper published in the British Medical Journal, we provided guidance for employers on assessing risk for healthcare workers during the Covid-19 pandemic. Risk management should involve training, measuring how well control measures are working, and learning from that experience. A risk management process should also involve consultation with staff. The pandemic has created an opportunity to improve safety in the workplace beyond covid-19, to consider cultural factors, and to ensure that all staff feel included and supported to raise concerns. How such processes have been conducted should also be evaluated to help improve risk management in the current pandemic and in any similar events in future.
DOI: https://doi.org/10.1136/bmj.n602