Associations between attainment of incentivized primary care indicators and incident sight‐threatening diabetic retinopathy
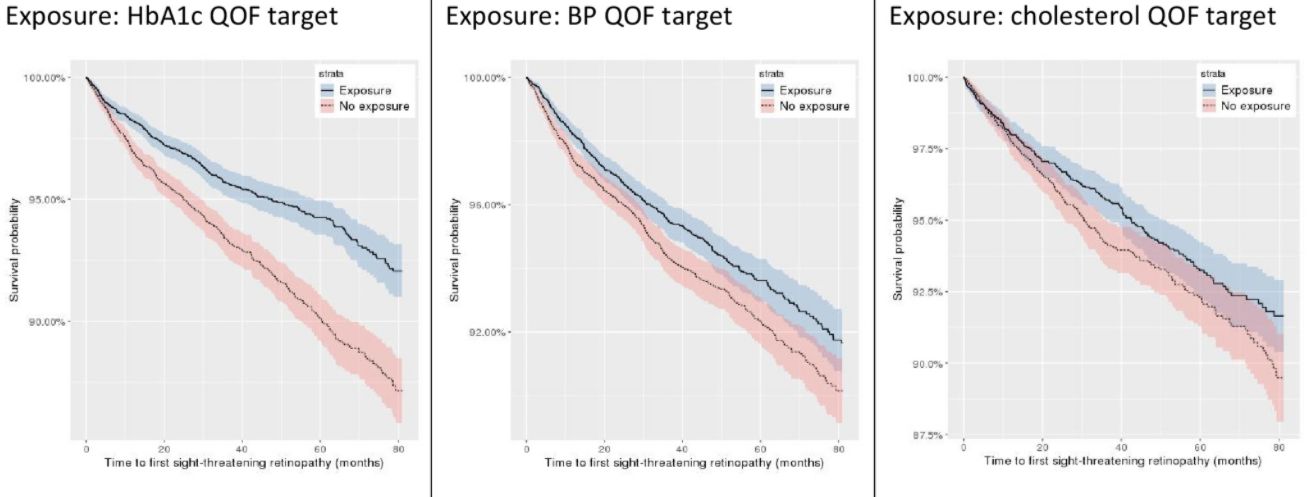
Our new study published in the journal Diabetes, Obesity and Metabolism shows a lower incidence of sight‐threatening diabetic retinopathy in people with type 2 diabetes who meet QOF targets for HBA1c, blood pressure and lipid control.
We aimed to examine the impact of attainment of primary care diabetes clinical indicators on progression to sight‐threatening diabetic retinopathy (STDR) among those with mild non‐proliferative diabetic retinopathy (NPDR).
We carried out a historical cohort study of 18,978 adults (43.63% female) diagnosed with type 2 diabetes before 1 April 2010 and mild NPDR before 1 April 2011 was conducted. The data were obtained from the UK Clinical Practice Research Datalink during 2010‐2017, provided by 330 primary care practices in England. Exposures included attainment of the Quality and Outcomes Framework HbA1c (≤59 mmol/mol [≤7.5%]), blood pressure (≤140/80 mmHg) and cholesterol (≤5 mmol/L) indicators in the financial year 2010‐2011, as well as the number of National Diabetes Audit processes completed in 2010‐2011. The outcome was time to incident STDR. Nearest neighbour propensity score matching was undertaken, and univariable and multivariable Cox proportional hazards models were then fitted using the matched samples. Concordance statistics were calculated for each model.
A total of 1037 (5.5%) STDR diagnoses were observed over a mean follow‐up of 3.6 (SD 2.0) years. HbA1c, blood pressure and cholesterol indicator attainment were associated with lower rates of STDR (adjusted hazard ratios [95% CI] 0.64 [0.55‐0.74; p < .001], 0.83 [0.72‐0.94; p = .005] and 0.80 [0.66‐0.96; p = .015], respectively).
Our findings provide support for meeting appropriate indicators for the management of type 2 diabetes in primary care to bring a range of benefits, including improved health outcomes—such as a reduction in the risk of STDR—for people with type 2 diabetes.
DOI: https://doi.org/10.1111/dom.14344