WATCCH: Widening Access to Community Careers in Healthcare 2019/20
by Dr Nicky Hawkins and Dr Nina Dutta
Since 2017, the Widening Access to Community Careers in Healthcare (WATCCH) programme has hosted over 100 individuals from diverse and disadvantaged backgrounds who are interested in a career in healthcare. The programme aims to support young people in making informed career choices, raise their aspirations and facilitate access to healthcare careers. Previous participants having gone on to take up offers on a wide range of healthcare-related degrees; amongst others, these include Dentistry, Nursing, Audiology, Biomedical Sciences, Pharmacy, Psychology, Radiography, Neuroscience and Medicine.
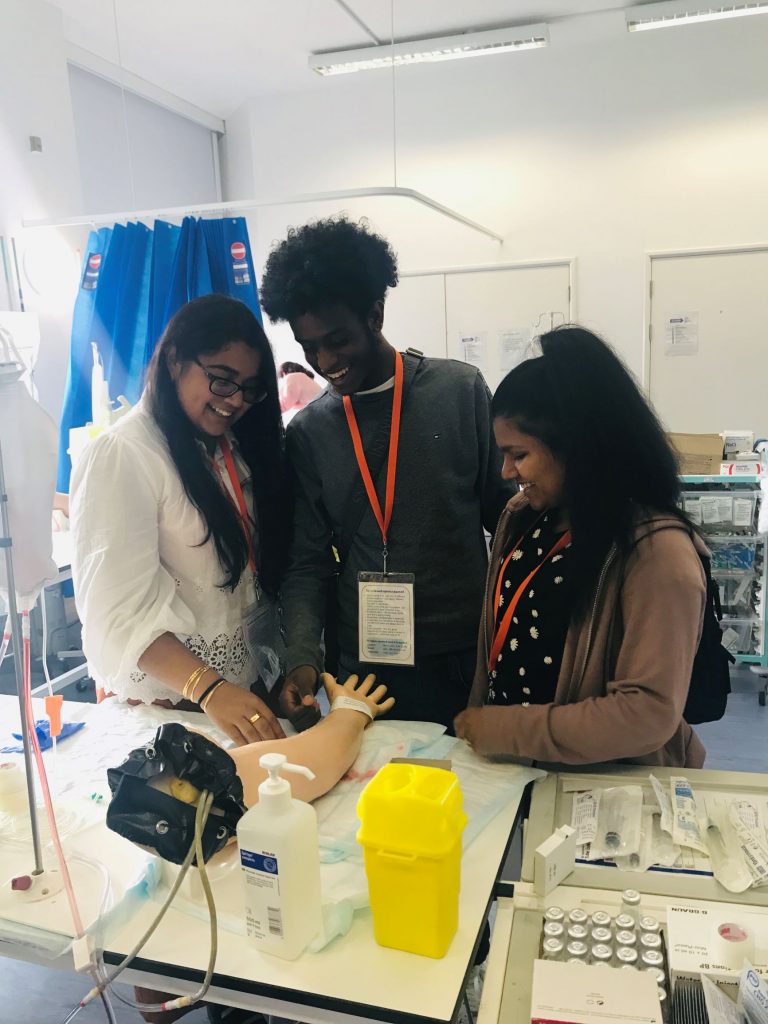
The 2019/20 WATCH programme has supported 40 students with primary care work experience and educational workshops, including multi-professional healthcare panel question and answer sessions and admissions workshops including personal statements and mock Multiple Mini Interview (MMI) circuits. This year’s programme has also included a mentoring scheme, whereby WATCCH participants are linked to current Imperial College School of Medicine (ICSM) student volunteers that have received training in coaching and mentoring. As the 2019/20 WATCCH programme comes to an end, our online closing event will focus on preparing students for the transition to life in higher education via a practical introduction to coaching, led by Dr Arti Maini, and talks spanning mentors’ ‘top tips’ on finances, accommodation, study skills and student welfare.
Looking ahead to 2020/21, we are committed to delivering a valuable WP programme despite the challenges posed by the COVID-19 pandemic. Applications are now open (until 27/06/2020) to eligible students as we begin to plan an innovative series of interactive online workshops accompanied by remote student mentoring. Using technology to our advantage we hope to expand the online programme to accommodate a higher number of students across the UK and also collaborate with a wider range of healthcare professionals. Evaluation of the programme also continues via the Higher Education Access Tracker (HEAT) and the Medical Education and Research Innovation Centre (MEdIC) based within Undergraduate Primary Care Education Team in the School of Public Health. As well as evaluating the programme from the perspective of student participants, we are also interested in the impact of near-peer WATCCH mentoring on the personal and professional development of mentors themselves.
Once again, we would like to thank all of the student participants, schools, teachers, and our Imperial WATCCH mentors for the enthusiasm and dedication that they bring to the programme.
Quote from student in the current WATCCH 2019/20 cohort:
“The WATCCH programme was fantastic in helping me secure medical school offers by firstly providing a week of general practice work experience. This was a valuable opportunity to shadow healthcare staff that could be included in my personal statement and discussed in the interview. There was a focus on reflective learning following the GP placement and then there was helpful support in the personal statement as well as practice MMI mock interviews. These sessions overall strengthened my medical school application by improving my confidence at every stage of the UCAS application process.”
For further information on WATCCH, please go to https://www.imperial.ac.uk/school-public-health/primary-care-and-public-health/teaching/widening-access-to-careers-in-community-healthcare/