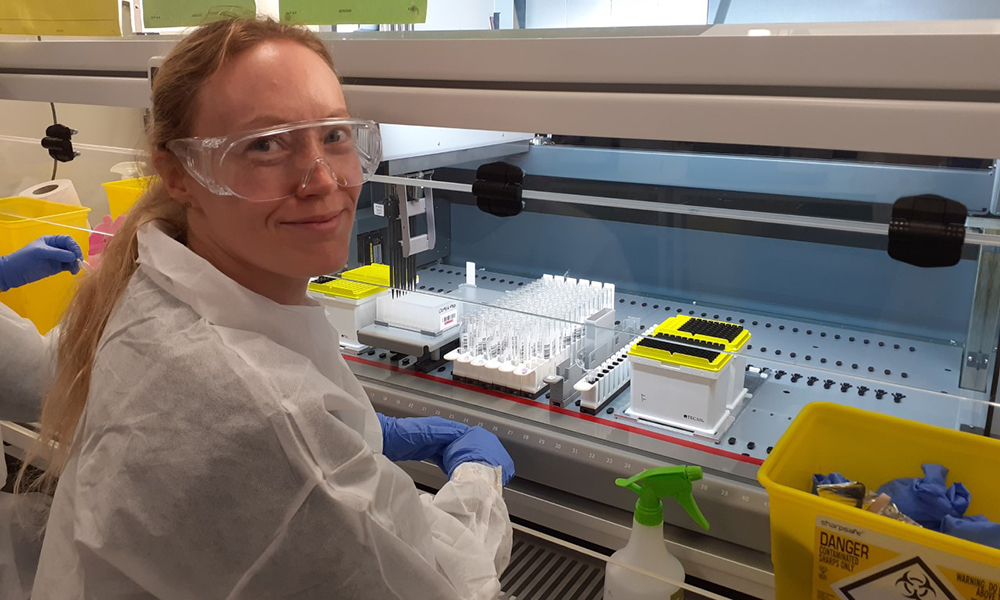
Dr Stephanie Ascough shares her experience of volunteering at the UK Biocentre in Milton Keynes, one of three Lighthouse Labs supporting large scale analysis of COVID-19 swabs from across the whole of the UK.
In mid-March, along with many of my colleagues at Imperial, I transitioned to working remotely, and our group sadly suspended all clinical research at the Hammersmith and St Mary’s Campuses. After the first few days of writing manuscripts in the garden though, I think many of us were surprised to realise how much we missed the lab, and I was no exception. On top of this was the feeling that, as an immunologist working with respiratory viruses, I had a skill set that would be valuable in the middle of a global pandemic. So, as soon as the call went out for volunteers to help with COVID-19 testing, I signed up. Within a week I heard back from the NIHR UK Biocentre in Milton Keynes. Shortly after this, in mid-April I found myself driving up an almost deserted M1, past signs reminding us to ‘Stay home, Save lives’ and restrict ourselves to ‘Essential travel only’.
 The UK Biocentre is located on the outskirts of Milton Keynes in a quiet industrial estate. Since March, this unobtrusive building has become one of three Lighthouse Labs (the others are in Glasgow and Alderley Park in Cheshire), the largest network of diagnostic testing facilities in British history, analysing COVID-19 swabs from across the UK. The UK Biocentre labs were uniquely placed to help in the testing efforts, as in normal life they are usually home to around 30 staff processing and archiving clinical samples from hospitals around the UK. However, the extent of the coronavirus pandemic required a massive scaling up of operations, with almost 200 volunteer research scientists recruited to work 12-hour shifts around the clock. The enormous amount of work also involved building and outfitting a brand new sample processing lab, larger than any single lab I’ve ever worked in. This, along with the existing UK Biocentre labs, has been filled with Microbiological Safety Cabinets (MSC), qPCR instruments and KingFisher RNA extraction instruments, all generously donated by academic labs from around the UK (including our own at Imperial).
The UK Biocentre is located on the outskirts of Milton Keynes in a quiet industrial estate. Since March, this unobtrusive building has become one of three Lighthouse Labs (the others are in Glasgow and Alderley Park in Cheshire), the largest network of diagnostic testing facilities in British history, analysing COVID-19 swabs from across the UK. The UK Biocentre labs were uniquely placed to help in the testing efforts, as in normal life they are usually home to around 30 staff processing and archiving clinical samples from hospitals around the UK. However, the extent of the coronavirus pandemic required a massive scaling up of operations, with almost 200 volunteer research scientists recruited to work 12-hour shifts around the clock. The enormous amount of work also involved building and outfitting a brand new sample processing lab, larger than any single lab I’ve ever worked in. This, along with the existing UK Biocentre labs, has been filled with Microbiological Safety Cabinets (MSC), qPCR instruments and KingFisher RNA extraction instruments, all generously donated by academic labs from around the UK (including our own at Imperial).
We were given a thorough staff induction on the first day, covering familiar areas such as health and safety, and human tissue authority legislation and ethics, as well as topics, perhaps less familiar to academics, such as diagnostic lab compliance standards. Subsequent days found us in the lab, where we were introduced to the existing staff and taken through the protocols. Every procedure is double-checked using a ‘buddy system’ to ensure compliance. In practice, this means we work in teams of two, with one individual collecting the sealed specimen transport bag and registering the unique identifying barcode on the bag and specimen tube containing the nasopharyngeal swab, on a computer system. This is then transferred to the scientist working in the MSC, who opens the sealed outer and inner bags and then the specimen tube, the viral transport medium within is pipetted into an allocated well of a 96-well plate, containing lysis buffer to inactivate the virus. All of which is witnessed by the second individual, with documentation at every stage. The UK Biocentre staff were at pains to emphasise that they didn’t doubt our ability to  run qPCR, rather this level of witnessing ensures that each sample is treated with the utmost care, and minimises chances of human error. To be honest, all the researchers I talked to were relieved to know a second person was checking each task, as all of us are keenly aware of the importance of accurate testing. The plate of inactivated virus is then taken to the KingFisher automated extraction instruments, and after several wash steps, familiar to anyone who has extracted RNA, the viral RNA is eluted into plates ready for the final steps, which involve the addition of the RNA along with PCR reagents to a qPCR plate by the automated Tecan PCR workstations. The genomic material is then amplified on one of 40 qPCR machines, to detect the presence of the virus. All of which means a result can be generated in less than 12 hours from the arrival of the swab at Milton Keynes.
run qPCR, rather this level of witnessing ensures that each sample is treated with the utmost care, and minimises chances of human error. To be honest, all the researchers I talked to were relieved to know a second person was checking each task, as all of us are keenly aware of the importance of accurate testing. The plate of inactivated virus is then taken to the KingFisher automated extraction instruments, and after several wash steps, familiar to anyone who has extracted RNA, the viral RNA is eluted into plates ready for the final steps, which involve the addition of the RNA along with PCR reagents to a qPCR plate by the automated Tecan PCR workstations. The genomic material is then amplified on one of 40 qPCR machines, to detect the presence of the virus. All of which means a result can be generated in less than 12 hours from the arrival of the swab at Milton Keynes.
In addition to the manual inactivation of the virus, I have spent quite a few shifts working with the high-throughput lysis Tecans. Along with the automated RNA exaction instruments and PCR Tecan workstations, these automated processes have allowed the UK Biocentre to exponentially increase the number of samples which can be processed every day (plus the robots are so satisfying to operate!). I feel lucky that my background in the Department of Infectious Disease at Imperial has left me comfortable working with clinical respiratory samples from influenza and RSV infected individuals, so all the biosafety and PPE requirements were second nature to me. Although, I don’t think any of us were quite prepared for the massive scale of the testing program; swabs are delivered constantly throughout the day and night by Royal Mail trucks and the lab is operating 24/7. The atmosphere has been amazing though, despite our team working from 8 pm to 8 am, the scientists are cheerful and determined. As is common with researchers in any lab, we’ve named all our equipment, with personal favourites being the PCR Tecan workstations named after the 5 Spice Girls, the KingFisher with the asset number KF007 (James Bond, obviously) and the lysis Tecan named ‘Florence the Machine’.
I feel very proud that, along with the clinicians and nurses at Imperial, I have been able to contribute to the UK’s effort to bring the coronavirus pandemic under control and save lives. This has been an amazing experience, working with such a diverse group of volunteer researchers and supportive management towards a single objective.
Now, I just have to convince the Section of Adult Infectious Disease we need one of those Tecans…
Dr Stephanie Ascough is a Research Associate in the Section of Adult Infectious Disease