New blog address
The Climate and Environment at Imperial blog has moved. Visit our new blog.
The Climate and Environment at Imperial blog has moved. Visit our new blog.
by Dr Kris Murray, Grantham Lecturer in Global Change Ecology
 Today the Lancet Commission on Health and Climate announced the release of their new report “2015 Lancet Commission on Health and Climate Change: Policy Responses to Protect Public Health”.
Today the Lancet Commission on Health and Climate announced the release of their new report “2015 Lancet Commission on Health and Climate Change: Policy Responses to Protect Public Health”.
Following a first report released in 2009, which concluded that “Climate change is the biggest global health threat of the 21st century”, today’s report has a proactive, positive take-home: “tackling climate change could be the greatest global health opportunity of the 21st century.”
Strategically released following the 68th World Health Assembly held last month and in the lead up to the UNFCCC’s COP21, to be held in Paris later this year, the report is the culmination of a second international (predominantly Chinese-European) working group assembled to assess the health impacts of climate change and to identify and accelerate effective mitigation and adaptation policies over the next 5 years.
The report provides 9 recommendations and delivers 1 promise:
Accompanying the launch of the report, the Lancet Commission on Health and Climate are holding a number of events around the world (including London, New York and Canberra), which will include speakers, panel discussions and an opportunity for Q&A from participants. The Health and Environment Alliance will also host a virtual launch event.
While the recommendations are not exactly breaking radical new ground, they do represent a welcome synthesis of the front-line evidence on the health impacts of climate change with a clear focus on solutions (the details of which make up the bulk of the report).
Perhaps more critically, they also crank up the volume of the voice of the health community at a critical time in the climate change arena – a voice that has a formidable track record of achievement in confronting other highly complex, trans-national, politically charged threats to health.
For further comment on the report, see the Lancet website.

Dr Kris Murray, Grantham Lecturer in Global Change Ecology
Our planet is ill. Ongoing loss and endangerment of species, degradation of marine and terrestrial ecosystems and their services, and manmade changes to the global climate are dramatic symptoms of a major decline in the planet’s environmental health.
In glaring contrast, human health has improved, in some cases radically. Decreases in malnutrition, mortality due to infectious diseases and infant mortality rates, accompanied by substantial increases in life expectancy, can be observed in every major region of the world.
So why is health winning a war, while the environment is losing one?
At a fundamental level, there is a huge difference in investment. Human health is a global priority and survival, healthiness and well-being are personal objectives for almost everyone. Preservation of the environment simply isn’t. Spending on global health, for example, is at least an order of magnitude greater than for environmental conservation.
But surely it’s not that simple. Ecosystem services and human health and well-being are supposed to be deeply interconnected, right? So how can we observe declining ecosystem services on the one hand and improving health and well-being on the other?
This question, sometimes referred to as “The Environmentalist’s Paradox”, has been used to suggest that the connections between environment and health are really not that important for the future of human welfare, despite some examples (such as the emergence of novel infectious diseases) that might suggest otherwise.
Alternative explanations for the Paradox do, however, exist.
One is that while total ecosystem services value may be falling, some services on which health is more fundamentally dependent continue to increase (e.g., provision of food).
Another is the suggestion that technological advances can and have resulted in a degree of de-coupling of health from nature.
Finally, time lags could mean that accrued and ongoing losses of ecosystem services and natural capital may yet toll health and well-being on much larger scales in the future, a factor that is thought to have contributed to previous civilization collapse.
At least one review of the evidence suggests that elements of each of these explanations remain plausible, while others are also presumably possible.
 To my mind, this means that compiling old and discovering new efficiencies in those areas of potential overlap between environmental and human health is looking increasingly like a very sensible strategy. In other words, there are still huge opportunities and a pressing need to identify and leverage health gains to help stem environmental losses. And vice versa.
To my mind, this means that compiling old and discovering new efficiencies in those areas of potential overlap between environmental and human health is looking increasingly like a very sensible strategy. In other words, there are still huge opportunities and a pressing need to identify and leverage health gains to help stem environmental losses. And vice versa.
In fact, from global targets on climate change mitigation and biodiversity conservation to disaster risk reduction and sustainable development, identifying potential and demonstrating genuine health ‘co-benefits’ is a growth industry. This approach is increasingly being used to find, and fund, mitigation and adaptation actions to address global environmental challenges.
The New Climate Institute, for example, estimates that more ambitious emissions reductions targets in the EU could prevent around 40,000 premature deaths per year from air pollution and create around 350,000 jobs in the domestic renewables sector.
Similarly, the UK’s Natural Capital Committee reports that investing in equitable access to green spaces would pay off with improved physical and mental health, generating savings of around £2.1 billion per year.
And perhaps a tad more abstractly, the Centre of Global Health Security highlights how successes in global environmental governance could be leveraged for better global health governance. This illustrates not only the potential breadth of co-beneficial links between environment and human health, but that not all of them necessarily require a natural capital accounting framework to take seriously (although this is clearly helping!).
So while the pursuit of win-win solutions for the environment and health in isolation is potentially an unhealthy obsession, when better to try than on World Environment Day? Working through the costs and trade-offs that typically follow can wait, at least until tomorrow.
Find out more on Grantham research on environmental change and health

The Climate and Environment at Imperial blog has moved. View this post on our new blog
By Dr Paul Parham, Honorary Lecturer in Infectious Disease Epidemiology
Many tropical diseases such as malaria, Chagas disease and dengue are transmitted to humans via mosquitoes and other carriers known as vectors. These vector-borne diseases continue to have a major impact on human health in the developing world: each year, more than a billion people become infected and around a million people die. In addition, around one in six cases of illness and disability worldwide arise from these diseases.
Malaria arguably continues to attract the most attention of all the vector-borne diseases by virtue of causing the greatest global disease burden. However, others such as dengue are not only resurgent in some regions, but threaten a vast proportion of the world’s population.
Climate change remains a substantial threat to future human health and since the behaviour of disease carriers like mosquitoes is known to be extremely sensitive to temperature and rainfall, it seems unquestionable that climate change will affect many, if not all, of these diseases. What is less clear, however, is the extent to which climate increases the risk of becoming infected in certain regions compared to other factors such as poverty or fragile health systems.
In addition, although the number of new cases of diseases such as malaria appears to be declining worldwide, it is still increasing in many regions for a variety of reasons; the continued spread of insecticide resistance, changes in land use, and difficulties in maintaining political interest pose considerable challenges. Which of these factors will be most influential over the coming decades remains up for debate and one that was raised in a special edition of Philosophical Transactions B.
The latest research, however, is clear and consistent in many of its findings. Different diseases, transmitted by different vectors, respond in different ways to changing weather and climate patterns. Climate change is very likely to favour an increase in the number of dengue cases worldwide, while many important mosquito populations that are able to transmit devastating diseases are changing in their distribution.
The latest maps show that many areas of Europe (including the UK) could become increasingly hospitable for mosquitoes that transmit dengue over the coming decades (the map below shows a projected change in suitable habitat for the Aedes albopictus mosquito). Similarly, other mosquito range expansions are likely to occur in the US and eastern Asia. If dengue and/or chikungunya are imported into these regions, there will be a considerable increase in the worldwide number of vulnerable individuals.
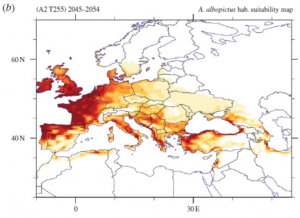
It is also clear that small changes in these so-called risk maps can have very large public health impacts. Tick-borne diseases (such as Lyme disease) are also predicted to expand in range as climate changes. Although, as before, plenty of other factors are likely to contribute, meaning that direct causation is very hard to attribute.
It is important to remember too that climate change is not just global warming; the latter refers to an increase in global mean temperatures, but there is also an overwhelming body of evidence demonstrating that rainfall is at least as important for many vector-borne diseases. Rainfall episodes have also been shown to provide a very good early-warning sign a few months in advance for outbreaks of West Nile Virus.
New research on African anti-malaria mosquito control programmes that involve spraying houses (to kill indoor mosquitoes) and distributing bed nets also shows that both temperature and rainfall can influence the degree to which programmes decrease new infections and, crucially, their cost-effectiveness. However, whether or not this is substantial enough to affect regional policy decisions about scaling up mosquito control programmes depends on factors such as how rapidly insecticide resistance emerges, the human immune response to malaria, and country-specific conditions.
In terms of malaria elimination in Africa, adopting the same approach in all affected regions is unlikely to be the best way forward. However, there is some new evidence to suggest that if efforts continue to be concentrated on scaling-up current intervention programmes in regions close to elimination, the longer-term effects of climate change will become far less important. Indeed, one of the most effective ways of protecting human health against climate change in the long-term is to further strengthen current disease control efforts.
As with the formulation of public health policies to deal with diseases such as Ebola, flu, and HIV, mathematical models are valuable tools that are widely used to make predictions about how different carrier-borne diseases are likely to respond to climatic changes. How reliable these predictions are is an important question and, like many areas of science, include unavoidable uncertainties. For example, people may change their behaviour and actions as climate change evolves – for example by migrating to other areas – which evidently makes forecasting more difficult.
New evidence has also shown that disease vectors may evolve in under a decade to changes in temperature, which conflicts with many current models that assume climate change only affects their ecology, not their evolution. Predictions that might be affected by climate change must therefore not only take account of these uncertainties, if they’re to be more reliable and useful, but also recognise that these predictions cannot strictly be disproved until the future arrives.
This remains a very active research field, but considerable progress in our understanding has been made over the last ten to 15 years. Better data on the links between vectors, diseases they carry and the environment is definitely required, as are better ways of quantifying disease risk for different populations and different diseases.
Many diseases have received very little attention so far on how climate change may affect future trends. One example is onchocerciasis (river blindness), for which tentative predictions suggest that we might expect substantial increases in the number of disease vectors in certain African regions over the coming decades.
Almost all models are currently based on single diseases, but many populations are unfortunately burdened with multiple diseases at any one time; understanding how climate change affects interactions between these diseases has attracted little attention to date.
One other important challenge for the field is the mismatch between the data current global climate models are able to provide and the information required by local public health officials to make more informed decisions; continued improvements in computing power are essential to progress. The predictions of our current models are not perfect and improvements in our understanding are certainly required.
To date, we have tended to react to disease outbreaks as they occur, but we need an increased focus on being more proactive; we cannot stop outbreaks of many of these diseases, but proactive risk management is less expensive (and more effective) than responding after a crisis. Ultimately, the challenge is not to address specific health risks due solely to climate change, but instead to ensure sustained progress is made towards decreasing the number of deaths and cases of these diseases for future generations.

This article was originally published on The Conversation.
Read the original article.
![]()
The Climate and Environment at Imperial blog has moved. View this post on our new blog
by Professor Paolo Vineis and Pauline Scheelbeek, School of Public Health

It is sometimes claimed that addressing climate change with proper policies is too expensive and could lead to a further decline in the economy. However, the co-benefits of implementation of climate change mitigation strategies for the health sector are usually overlooked. The synergy between policies for climate change mitigation in sectors such as energy use (e.g. for heating), agriculture, food production and transportation may have overall benefits that are much greater than the sum of single interventions (Haines et al, 2009). Here we describe a few examples of climate change mitigation strategies that have important co-benefits for global health.
The transportation sector is often the single largest source of greenhouse gas emissions in urban areas. Policy makers have tried to reduce these emissions by discouraging car travel and promoting other means of (active) transport. Active transport, such as cycling and walking, increases daily physical activity. Physical inactivity is one of the leading causes of non-communicable diseases all over the world. It has been estimated that the combination of active travel and lower-emission motor vehicles would give large health benefits, notably from a reduction in the number of years of life lost from coronary heart disease (10-19% in London, 11-25% in Delhi according to Woodcock et al, 2009). Also obesity, which is increasing dramatically all over the world, particularly in children, could effectively be reduced by a more active lifestyle. A 30-minute walk per day could – on many occasions – be enough to even out slight caloric excess.
Improving heating and cooking systems – for example by making them more efficient – reduces energy consumption. Improved models of stoves (electrical vs biomass) allow a 15-times reduction in the emission of particles and other pollutants, thus contributing to decreased emissions in the atmosphere. Especially in developing countries – where old stoves are common – these improvements could also have a considerable positive impact on health: cooking on simple wood or coal stoves currently forms a major source of indoor pollution and increases risk of certain chronic diseases, such as chronic obstructive pulmonary disease (COPD). The potential effectiveness of this strategy was shown by Wilkinson et al: they calculated that if 150 million low-emission cookstoves were introduced in India, this could lead to the prevention of an estimated 1.3 million deaths from COPD and hundreds of thousands of deaths from other diseases such as coronary heart disease (Wilkinson, et al 2009). Air pollution is one of the biggest environmental causes of death worldwide, with household air pollution accounting for about 3·5-4 million deaths every year (Gordon et al, 2014).
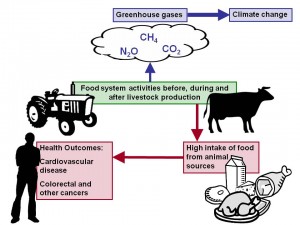 Meat production is highly inefficient energetically: it requires an extremely high use of water and land per unit of meat. One fifth of all greenhouse gases worldwide are related to methane production from livestock farms. Reduction of meat intake by consumers would lower meat production and is therefore often promoted as climate change mitigation strategy. The figure shows that a high intake of meat is also associated with increased disease risk, in particular for certain cancers and cardiovascular disease (WCRF, 2007). Reduced meat consumption would therefore also have a major impact on public health. It has been estimated that a 30% reduction in livestock production in the UK would reduce cardiovascular deaths by 15% (Friel et al, 2009).
Meat production is highly inefficient energetically: it requires an extremely high use of water and land per unit of meat. One fifth of all greenhouse gases worldwide are related to methane production from livestock farms. Reduction of meat intake by consumers would lower meat production and is therefore often promoted as climate change mitigation strategy. The figure shows that a high intake of meat is also associated with increased disease risk, in particular for certain cancers and cardiovascular disease (WCRF, 2007). Reduced meat consumption would therefore also have a major impact on public health. It has been estimated that a 30% reduction in livestock production in the UK would reduce cardiovascular deaths by 15% (Friel et al, 2009).
Non-renewable energy production, for example coal burning, is a major contributor to worldwide greenhouse gas emissions. Many countries have adopted policies to reduce polluting energy production and stimulate production of (renewable) energy through cleaner sources. For example, since 2000, the government in the Chinese Shanxi province has promoted several initiatives (including factory shutdowns) with the goal of reducing coal burning emissions. The annual average particulate matter (PM10) concentrations decreased from 196 μg/m3 in 2001 to 89 μg/m3 in 2010, which – as a matter of fact – is still very high for Western standards. It has been estimated that the DALYs (Disability-Adjusted Life Years) lost in Shanxi had decreased by 56.92% as a consequence of the measures (Tang et al, 2014). The IPCC 5th assessment report stresses that the main health co-benefits from climate change mitigation policies come from substituting polluting sources of energy for renewable and cleaner sources, with a considerable effect on the improvement of air quality.
The co-benefits from climate change mitigation for the health sector have not yet been completely identified and quantified. The topic does not appear on the priority list of political discourse: relevant sectors, including those involved in non-communicable disease prevention (Pearce et al, 2014), transportation, agriculture, food production and climate change (Alleyne et al, 2013), still work separately, while collaboration would improve the synergy between health improvement and climate change mitigation and maximise benefits for both.
References
Alleyne G, Binagwaho A, Haines A, Jahan S, Nugent R, Rojhani A, Stuckler D; Lancet NCD Action Group. Embedding non-communicable diseases in the post-2015 development agenda. Lancet. 2013 Feb 16;381(9866):566-74. doi: 10.1016/S0140-6736(12)61806-6
Friel S, Dangour AD, Garnett T, Lock K, Chalabi Z, Roberts I, Butler A, Butler CD, Waage J, McMichael AJ, Haines A. Public health benefits of strategies to reduce greenhouse-gas emissions: food and agriculture. Lancet 2009; 374: 2016-25.
Gordon SB, Bruce NG, Grigg J, Hibberd PL, Kurmi OP, Lam KB, Mortimer K, Asante KP, Balakrishnan K, Balmes J, Bar-Zeev N, Bates MN, Breysse PN, Buist S, Chen Z, Havens D, Jack D, Jindal S, Kan H, Mehta S, Moschovis P, Naeher L, Patel A, Perez-Padilla R, Pope D, Rylance J, Semple S, Martin WJ 2nd. Respiratory risks from household air pollution in low and middle income countries. Lancet Respir Med. 2014 Oct;2(10):823-60. doi: 10.1016/S2213-2600(14)70168-7
Haines A, McMichael AJ, Smith KR, Roberts I, Woodcock J, Markandya A, Armstrong BG, Campbell-Lendrum D, Dangour AD, Davies M, Bruce N, Tonne C, Barrett M, Wilkinson P. Public health benefits of strategies to reduce greenhouse-gas emissions: overview and implications for policy makers. Lancet. 2009 Dec 19;374(9707):2104-14. doi: 10.1016/S0140-6736(09)61759-1. Epub 2009 Nov 26.
Pearce N, Ebrahim S, McKee M, Lamptey P, Barreto ML, Matheson D, Walls H, Foliaki S, Miranda J, Chimeddamba O, Marcos LG, Haines A, Vineis P. The road to 25×25: how can the five-target strategy reach its goal? Lancet Glob Health. 2014 Mar;2(3):e126-8. doi: 10.1016/S2214-109X(14)70015-4.
Tang D, Wang C, Nie J, Chen R, Niu Q, Kan H, Chen B, Perera F; Taiyuan CDC. Health benefits of improving air quality in Taiyuan, China. Environ Int. 2014 Dec;73:235-42. doi: 10.1016/j.envint.2014.07.016. Epub 2014 Aug 27.
Wilkinson P, Smith KR, Davies M, Adair H, Armstrong BG, Barrett M, Bruce N, Haines A, Hamilton I, Oreszczyn T, Ridley I, Tonne C and Chalabi Z. Public health benefits of strategies to reduce greenhouse-gas emissions: household energy. 2009. The Lancet, 374: 9705 (P1917 – 29)
World Cancer Research Fund. Recommendations Booklet. Available from: http://www.wcrf.org/
Woodcock J, Edwards P, Tonne C, Armstrong BG, Ashiru O, Banister D, Beevers S, Chalabi Z, Chowdhury Z, Cohen A, Franco OH, Haines A, Hickman R, Lindsay G, Mittal I, Mohan D, Tiwari G, Woodward A, Roberts I. Public health benefits of strategies to reduce greenhouse-gas emissions: urban land transport. Lancet. 2009 Dec 5;374(9705):1930-43. doi: 10.1016/S0140-6736(09)61714-1. Epub 2009 Nov 26.