
The Climate and Environment at Imperial blog has moved. View this post on our new blog
By Dr Paul Parham, Honorary Lecturer in Infectious Disease Epidemiology
Many tropical diseases such as malaria, Chagas disease and dengue are transmitted to humans via mosquitoes and other carriers known as vectors. These vector-borne diseases continue to have a major impact on human health in the developing world: each year, more than a billion people become infected and around a million people die. In addition, around one in six cases of illness and disability worldwide arise from these diseases.
Malaria arguably continues to attract the most attention of all the vector-borne diseases by virtue of causing the greatest global disease burden. However, others such as dengue are not only resurgent in some regions, but threaten a vast proportion of the world’s population.
Climate change remains a substantial threat to future human health and since the behaviour of disease carriers like mosquitoes is known to be extremely sensitive to temperature and rainfall, it seems unquestionable that climate change will affect many, if not all, of these diseases. What is less clear, however, is the extent to which climate increases the risk of becoming infected in certain regions compared to other factors such as poverty or fragile health systems.
In addition, although the number of new cases of diseases such as malaria appears to be declining worldwide, it is still increasing in many regions for a variety of reasons; the continued spread of insecticide resistance, changes in land use, and difficulties in maintaining political interest pose considerable challenges. Which of these factors will be most influential over the coming decades remains up for debate and one that was raised in a special edition of Philosophical Transactions B.
Changes in risk
The latest research, however, is clear and consistent in many of its findings. Different diseases, transmitted by different vectors, respond in different ways to changing weather and climate patterns. Climate change is very likely to favour an increase in the number of dengue cases worldwide, while many important mosquito populations that are able to transmit devastating diseases are changing in their distribution.
The latest maps show that many areas of Europe (including the UK) could become increasingly hospitable for mosquitoes that transmit dengue over the coming decades (the map below shows a projected change in suitable habitat for the Aedes albopictus mosquito). Similarly, other mosquito range expansions are likely to occur in the US and eastern Asia. If dengue and/or chikungunya are imported into these regions, there will be a considerable increase in the worldwide number of vulnerable individuals.
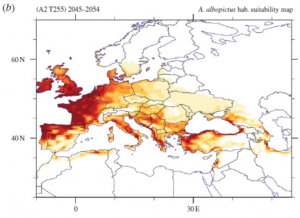
It is also clear that small changes in these so-called risk maps can have very large public health impacts. Tick-borne diseases (such as Lyme disease) are also predicted to expand in range as climate changes. Although, as before, plenty of other factors are likely to contribute, meaning that direct causation is very hard to attribute.
It is important to remember too that climate change is not just global warming; the latter refers to an increase in global mean temperatures, but there is also an overwhelming body of evidence demonstrating that rainfall is at least as important for many vector-borne diseases. Rainfall episodes have also been shown to provide a very good early-warning sign a few months in advance for outbreaks of West Nile Virus.
New research on African anti-malaria mosquito control programmes that involve spraying houses (to kill indoor mosquitoes) and distributing bed nets also shows that both temperature and rainfall can influence the degree to which programmes decrease new infections and, crucially, their cost-effectiveness. However, whether or not this is substantial enough to affect regional policy decisions about scaling up mosquito control programmes depends on factors such as how rapidly insecticide resistance emerges, the human immune response to malaria, and country-specific conditions.
In terms of malaria elimination in Africa, adopting the same approach in all affected regions is unlikely to be the best way forward. However, there is some new evidence to suggest that if efforts continue to be concentrated on scaling-up current intervention programmes in regions close to elimination, the longer-term effects of climate change will become far less important. Indeed, one of the most effective ways of protecting human health against climate change in the long-term is to further strengthen current disease control efforts.
Mathematical models
As with the formulation of public health policies to deal with diseases such as Ebola, flu, and HIV, mathematical models are valuable tools that are widely used to make predictions about how different carrier-borne diseases are likely to respond to climatic changes. How reliable these predictions are is an important question and, like many areas of science, include unavoidable uncertainties. For example, people may change their behaviour and actions as climate change evolves – for example by migrating to other areas – which evidently makes forecasting more difficult.
New evidence has also shown that disease vectors may evolve in under a decade to changes in temperature, which conflicts with many current models that assume climate change only affects their ecology, not their evolution. Predictions that might be affected by climate change must therefore not only take account of these uncertainties, if they’re to be more reliable and useful, but also recognise that these predictions cannot strictly be disproved until the future arrives.
This remains a very active research field, but considerable progress in our understanding has been made over the last ten to 15 years. Better data on the links between vectors, diseases they carry and the environment is definitely required, as are better ways of quantifying disease risk for different populations and different diseases.
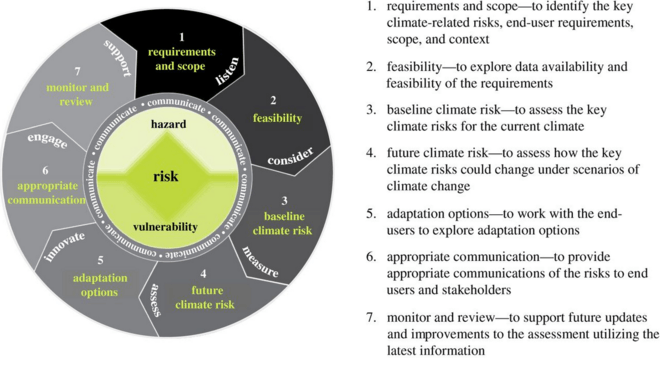
Seven steps to understanding climate impacts and assessing risks.
Philosophical Transactions B
Future challenges
Many diseases have received very little attention so far on how climate change may affect future trends. One example is onchocerciasis (river blindness), for which tentative predictions suggest that we might expect substantial increases in the number of disease vectors in certain African regions over the coming decades.
Almost all models are currently based on single diseases, but many populations are unfortunately burdened with multiple diseases at any one time; understanding how climate change affects interactions between these diseases has attracted little attention to date.
One other important challenge for the field is the mismatch between the data current global climate models are able to provide and the information required by local public health officials to make more informed decisions; continued improvements in computing power are essential to progress. The predictions of our current models are not perfect and improvements in our understanding are certainly required.
To date, we have tended to react to disease outbreaks as they occur, but we need an increased focus on being more proactive; we cannot stop outbreaks of many of these diseases, but proactive risk management is less expensive (and more effective) than responding after a crisis. Ultimately, the challenge is not to address specific health risks due solely to climate change, but instead to ensure sustained progress is made towards decreasing the number of deaths and cases of these diseases for future generations.

This article was originally published on The Conversation.
Read the original article.
![]()